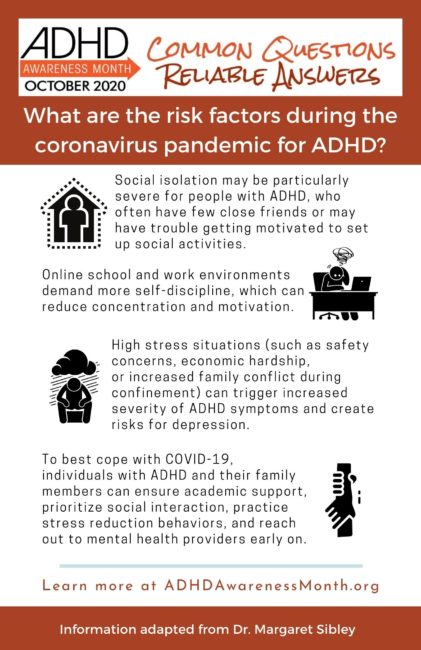
Emerging studies from the COVID-19 pandemic show that ADHD symptom severity appears to be increasing during this global event. Several factors may be to blame. First, students with ADHD must adjust to low-structure, online learning platforms. These school environments demand more self-discipline than regular school, which can make concentration and motivation very challenging. For older high school and college students with ADHD, disengaging from virtual school may pave a slippery path towards formal dropout. Warning signs include a build-up of missing work, avoiding virtual class meetings, and slipping grades.
Second, social isolation is a known consequence of COVID-19 and is a risk factor for depression and suicide. During COVID-19, social isolation may be particularly severe for people with ADHD, who often have few close friends or may have trouble getting motivated to set-up social activities. On top of this concern, increased ADHD symptoms can be triggered by high stress situations. COVID-19 brings stressors that include safety concerns, economic hardship, and increased family conflict during confinement. In addition to worsening ADHD symptoms, ongoing stress exposure can also create risks for depression. To prevent these concerns, individuals with ADHD and their family members can:
- ensure that proper academic supports are in place at school,
- prioritize social interaction (even if it means getting creative) during COVID-19,
- practice stress reduction behaviors such as outdoor and physical activity, spending positive time with loved ones, and practicing favorite hobbie, and
- reach out to mental health providers early on if you notice signs of emerging school disengagement or depression.
Both mental health therapy and medication can support children, adolescents, and adults with ADHD through these challenging times.
About the Author

Margaret H. Sibley, Ph.D. is Associate Professor of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine and a Licensed Clinical Psychologist at Seattle Children’s Hospital. Her research is focused on ADHD in adolescence and young adulthood.
References
- Behar‐Zusman, V., Chavez, J. V., & Gattamorta, K. (2020). Developing a measure of the impact of COVID-19 social distancing on household conflict and cohesion. Family Process, 59(3), 1045–1059.
- Becker, S. P., Breaux, R., Cusick, C. N., Dvorsky, M. R., Marsh, N. P., Sciberras, E., & Langberg, J. M. (in press). Remote learning during COVID-19: Examining school practices, service continuation, and difficulties for adolescents with and without ADHD. Journal of Adolescent Health.
- Bobo, E., Lin, L., Acquaviva, E., Caci, H., Franc, N., Gamon, L., … & Purper-Ouakil, D. (2020). How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak?. L’encephale.
- Cortese, S., Asherson, P., Sonuga-Barke, E., Banaschewski, T., Brandeis, D., Buitelaar, J., Coghill, D., Daley, D., Danckaerts, M., Dittmann, R. W., Doepfner, M., Ferrin, M., Hollis, C., Holtmann, M., Konofal, E., Lecendreux, M., Santosh, P., Rothenberger, A., Soutullo, C., … Simonoff, E. (2020). ADHD management during the COVID-19 pandemic: Guidance from the European ADHD Guidelines Group. The Lancet Child & Adolescent Health, 4(6), 412–414. https://doi.org/10.1016/S2352-4642(20)30110-3
- Courtet, P., Olié, E., Debien, C., & Vaiva, G. (2020). Keep socially (but not physically) connected and carry on: Preventing suicide in the age of COVID-19. Journal of clinical psychiatry, 81(3), e20com13370-e20com13370.
- Eadeh, H.-M., Bourchtein, E., Langberg, J. M., Eddy, L. D., Oddo, L., Molitor, S. J., & Evans, S. W. (2017). Longitudinal evaluation of the role of academic and social impairment and parent-adolescent conflict in the development of depression in adolescents with ADHD. Journal of Child and Family Studies, 26(9), 2374–2385. https://doi.org/10.1007/s10826-017-0768-7
- Ellis, W. E., Dumas, T. M., & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 52(3), 177.
- Hall-Lande, J. A., Eisenberg, M. E., Christenson, S. L., & Neumark-Sztainer, D. (2007). Social isolation, psychological health, and protective factors in adolescence. Adolescence, 42(166), 265-. Gale Academic OneFile.
- Hartman, C. A., Rommelse, N., van der Klugt, C. L., Wanders, R. B. K., & Timmerman, M. E. (2019). Stress exposure and the course of ADHD from childhood to young adulthood: Comorbid severe emotion dysregulation or mood and anxiety problems. Journal of Clinical Medicine, 8(11), 1824. https://doi.org/10.3390/jcm8111824
- Horesh, D., & Brown, A. D. (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 331.
- Zhang, J., Shuai, L., Yu, H., Wang, Z., Qiu, M., Lu, L., … & Chen, R. (2020). Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian journal of psychiatry, 51, 102077.