It appears that adults with ADHD have 4-5 times the risk of developing a Substance Use Disorder than those who don’t have ADHD (1, 2). Both our genes and our life experiences probably contribute to this elevated risk. (3-7).
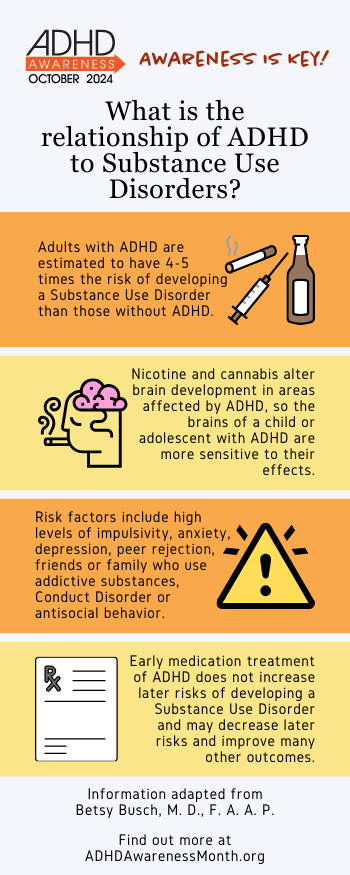
Children and adolescents with ADHD initiate nicotine and cannabis use earlier than their peers without ADHD, and become dependent faster(8). Nicotine and cannabis alter brain development in areas affected by ADHD, so the brain of a child or adolescent with ADHD is more sensitive to the effects of these addictive substances (9, 10). Younger initiation of cannabis use and prescription drug misuse have both been associated with higher rates and faster development of Substance Use Disorders (11). Other factors that further magnify the risk of developing a substance use disorder include:
- high levels of impulsivity
- anxiety, depression and other psychiatric conditions which occur in ~80% of people with ADHD
- peer rejection
- friends who use addictive or illicit substances
- family members with problematic drinking/substance use
- Conduct Disorder or antisocial behavior
Because early experimentation can begin before adolescence, prevention should begin early. Family discussions about avoiding nicotine, cannabis and alcohol should begin by age 9-10, and avoidance/deferral should continue throughout adolescence/young adulthood, when substance misuse becomes most problematic. Teach children/adolescents to take all medications, especially ADHD medications, only as prescribed.
Early medication treatment of ADHD does not increase later risks of developing a Substance Use Disorder. In fact, early and sustained treatment of ADHD may decrease these later risks, and may improve many other outcomes (12-14). It’s also important to treat any co-morbid psychiatric disorders.
If problematic use does develop, treatment programs that address both substance misuse and ADHD/other co-morbid conditions can be very helpful (15-17). The course of Substance Use Disorders in those with ADHD is often longer, more complex, and more likely to reflect misuse of multiple substances(18). Although relapses are common, continued recovery efforts ultimately can be successful.
About the Author

Betsy Busch, M. D., F. A. A. P. is an Associate Clinical Professor of Pediatrics at Tufts University School of Medicine. She is a well-known ADHD specialist and thought leader in the field, and is currently Treasurer of APSARD.
References:
1. Hartman CA, Larsson H, Vos M, Bellato A, Libutzki B, Solberg BS, Chen Q, Du Rietz E, Mostert JC, Kittel-Schneider S, Cormand B, Ribases M, Klungsoyr K, Haavik J, Dalsgaard S, Cortese S, Faraone SV, Reif A. Anxiety, mood, and substance use disorders in adult men and women with and without attention-deficit/hyperactivity disorder: A substantive and methodological overview. Neurosci Biobehav Rev. 2023;151:105209.
2. Rohner H, Gaspar N, Philipsen A, Schulze M. Prevalence of Attention Deficit Hyperactivity Disorder (ADHD) among Substance Use Disorder (SUD) Populations: Meta-Analysis. Int J Environ Res Public Health. 2023;20(2).
3. Chen W, Epstein A, Toner M, Murphy N, Rudaizky D, Downs J. Enabling successful life engagement in young people with ADHD: new components beyond adult models of recovery. Disabil Rehabil. 2023;45(14):2288-2300.
4. Tang S, Ports KA, Zhang K, Lin HC. Adverse childhood experiences, internalizing/externalizing symptoms, and associated prescription opioid misuse: A mediation analysis. Prev Med. 2020;134:106034.
5. Kendler KS, Ohlsson H, Sundquist J, Sundquist K. The patterns of family genetic risk scores for eleven major psychiatric and substance use disorders in a Swedish national sample. Transl Psychiatry. 2021;11(1):326.
6. Garcia-Marin LM, Campos AI, Cuellar-Partida G, Medland SE, Kollins SH, Renteria ME. Large-scale genetic investigation reveals genetic liability to multiple complex traits influencing a higher risk of ADHD. Sci Rep. 2021;11(1):22628.
7. Wimberley T, Agerbo E, Horsdal HT, Ottosen C, Brikell I, Als TD, Demontis D, Borglum AD, Nordentoft M, Mors O, Werge T, Hougaard D, Bybjerg-Grauholm J, Hansen MB, Mortensen PB, Thapar A, Riglin L, Langley K, Dalsgaard S. Genetic liability to ADHD and substance use disorders in individuals with ADHD. Addiction. 2020;115(7):1368-1377.
8. Ozgen H, Spijkerman R, Noack M, Holtmann M, Schellekens ASA, van de Glind G, Banaschewski T, Barta C, Begeman A, Casas M, Crunelle CL, Daigre Blanco C, Dalsgaard S, Demetrovics Z, den Boer J, Dom G, Eapen V, Faraone SV, Franck J, Gonzalez RA, Grau-Lopez L, Groenman AP, Hemphala M, Icick R, Johnson B, Kaess M, Kapitany-Foveny M, Kasinathan JG, Kaye SS, Kiefer F, Konstenius M, Levin FR, Luderer M, Martinotti G, Matthys FIA, Meszaros G, Moggi F, Munasur-Naidoo AP, Post M, Rabinovitz S, Ramos-Quiroga JA, Sala R, Shafi A, Slobodin O, Staal WG, Thomasius R, Truter I, van Kernebeek MW, Velez-Pastrana MC, Vollstadt-Klein S, Vorspan F, Young JT, Yule A, van den Brink W, Hendriks V. International Consensus Statement for the Screening, Diagnosis, and Treatment of Adolescents with Concurrent Attention-Deficit/Hyperactivity Disorder and Substance Use Disorder. Eur Addict Res. 2020;26(4-5):223-232.
9. Kandel ER, Kandel DB. Shattuck Lecture. A molecular basis for nicotine as a gateway drug. N Engl J Med. 2014.
10. Williams AR. Cannabis as a Gateway Drug for Opioid Use Disorder. J Law Med Ethics. 2020;48(2):268-274.
11. Volkow ND, Han B, Einstein EB, Compton WM. Prevalence of Substance Use Disorders by Time Since First Substance Use Among Young People in the US. JAMA Pediatr. 2021;175(6):640-643.
12. Wilens TE, Woodward DW, Ko JD, Berger AF, Burke C, Yule AM. The Impact of Pharmacotherapy of Childhood-Onset Psychiatric Disorders on the Development of Substance Use Disorders. J Child Adolesc Psychopharmacol. 2022;32(4):200-214.
13. Kennedy TM, Molina BSG. Translating the nuanced risk for substance use among adolescents treated for attention-deficit/hyperactivity disorder (ADHD) into clinical practice: a commentary on McCabe et al. (2023). J Child Psychol Psychiatry. 2023.
14. Boland H, DiSalvo M, Fried R, Woodworth KY, Wilens T, Faraone SV, Biederman J. A literature review and meta-analysis on the effects of ADHD medications on functional outcomes. J Psychiatr Res. 2020;123:21-30.
15. Kast KA, Rao V, Wilens TE. Pharmacotherapy for Attention-Deficit/Hyperactivity Disorder and Retention in Outpatient Substance Use Disorder Treatment: A Retrospective Cohort Study. J Clin Psychiatry. 2021;82(2):20m13598.
16. Tardelli V, Xu KY, Bisaga A, Levin FR, Fidalgo TM, Grucza RA. Prescription amphetamines in people with opioid use disorder and co-occurring psychostimulant use disorder initiating buprenorphine: an analysis of treatment retention and overdose risk. BMJ Ment Health. 2023;26(1).
17. van Emmerik-van Oortmerssen K, Vedel E, Kramer FJ, Blankers M, Dekker JJM, van den Brink W, Schoevers RA. Integrated cognitive behavioral therapy for ADHD in adult substance use disorder patients: Results of a randomized clinical trial. Drug Alcohol Depend. 2019;197:28-36.
18. Fatseas M, Hurmic H, Serre F, Debrabant R, Daulouede JP, Denis C, Auriacombe M. Addiction severity pattern associated with adult and childhood Attention Deficit Hyperactivity Disorder (ADHD) in patients with addictions. Psychiatry Res. 2016;246:656-662.
